MAXILLOFACIAL SURGERY
Facial Trauma
Facial Trauma Treatment By Best Maxillofacial Surgeon In Surat
Facial trauma is any injury of the face and upper jaw bone (maxilla).
Causes
As per our expert maxillofacial surgeon blunt or penetrating trauma can cause injury to the area of the face that includes the upper jaw, lower jaw, cheek, nose, or forehead. Common causes of injury to the face include :
- Automobile accidents
- Penetrating injuries
- Violence
Symptoms
- Changes in sensation and feeling over the face
- Deformed or uneven face or facial bones
- Difficulty breathing through the nose due to swelling and bleeding
- Double vision
- Missing teeth
- Swelling around the eyes that may cause vision problems
Exams and Tests The maxillofacial surgeon will perform a physical exam, which may show :
- Bleeding from the nose, eyes, or mouth, or nasal blockage
- Breaks in the skin (lacerations)
- Bruising around the eyes or widening of the distance between the eyes, which may mean injury to the bones between the eye sockets
According to our maxillofacial surgeon the following may suggest bone fractures :
- Abnormal sensations on the cheek and irregularities that can be felt
- An upper jaw that moves when the head is still
- A CT scan of the head may be done.
Best treatment by our maxillofacial surgeon in Surat
Patients who cannot function normally or who have significant deformity will need surgery. The goal of treatment is to:
- Control bleeding
- Create a clear airway
- Fix broken bone segments with titanium plates and screws
- Leave the fewest scars possible
- Rule out other injuries
- Treat the fracture
Treatment should be immediate, as long as the person is stable and there are no neck fractures or life-threatening injuries.
Outlook (Prognosis) Patients generally do very well with proper treatment. You will probably look different than you did before your injury. You may need to have more surgery 6 - 12 months later.
Possible Complications
General complications include, but are not limited to:
- Bleeding
- Uneven face
- Infection
- Brain and nervous system problems
- Numbness or weakness
- Loss of vision or double vision
Fill up the query form or call us to make an appointment for maxillofacial surgeon in Surat.
Make an appointment
Cleft Lip/Palate

Cleft lip and cleft palate are facial and oral malformations that occur very early in pregnancy, while the baby is developing inside the mother. Clefting results when there is not enough tissue in the mouth or lip area, and the tissue that is available does not join together properly.
A cleft lip is a physical split or separation of the two sides of the upper lip and appears as a narrow opening or gap in the skin of the upper lip. This separation often extends beyond the base of the nose and includes the bones of the upper jaw and/or upper gum.
A cleft palate is a split or opening in the roof of the mouth. A cleft palate can involve the hard palate (the bony front portion of the roof of the mouth), and/or the soft palate (the soft back portion of the roof of the mouth). Cleft lip and cleft palate can occur on one or both sides of the mouth. Because the lip and the palate develop separately, it is possible to have a cleft lip without a cleft palate, a cleft palate without a cleft lip, or both together.
Who Gets Cleft Lip And Cleft Palate?
Cleft lip, with or without cleft palate, affects one in 700 babies annually, and is the fourth most common birth defect in the U.S. Clefts occur more often in children of Asian, Latino, or Native American descent. Compared with girls, twice as many boys have a cleft lip, both with and without a cleft palate. However, compared with boys, twice as many girls have cleft palate without a cleft lip.
What Causes A Cleft Lip And Cleft Palate?
In most cases, the cause of cleft lip and cleft palate is unknown. These conditions cannot be prevented. Most scientists believe clefts are due to a combination of genetic and environmental factors. There appears to be a greater chance of clefting in a newborn if a sibling, parent, or relative has had the problem.
Another potential cause may be related to a medication a mother may have taken during her pregnancy. Some drugs may cause cleft lip and cleft palate. Among them: anti-seizure/anticonvulsant drugs, acne drugs containing Cutaneous, and methotrexate, a drug commonly used for treating cancer, arthritis, and psoriasis.
Cleft lip and cleft palate may also occur as a result of exposure to viruses or chemicals while the fetus is developing in the womb.
In other situations, cleft lip and cleft palate may be part of another medical condition.
How Are Cleft Lip And Cleft Palate Diagnosed?
Because clefting causes very obvious physical changes, a cleft lip or cleft palate is easy to diagnose. Prenatal ultrasound can sometimes determine if a cleft exists in an unborn child. If the clefting has not been detected in an ultrasound prior to the baby's birth, a physical exam of the mouth, nose, and palate confirms the presence of cleft lip or cleft palate after a child's birth. Sometimes diagnostic testing may be conducted to determine or rule out the presence of other abnormalities.
What's The Treatment For Cleft Lip And Cleft Palate?
A cleft lip may require one or two surgeries depending on the extent of the repair needed. The initial surgery is usually performed by the time a baby is 3 months old.
Repair of a cleft palate often requires multiple surgeries over the course of 18 years. The first surgery to repair the palate usually occurs when the baby is between 6 and 12 months old. The initial surgery creates a functional palate, reduces the chances that fluid will develop in the middle ears, and aids in the proper development of the teeth and facial bones.
Children with a cleft palate may also need a bone graft when they are about 8 years old to fill in the upper gum line so that it can support permanent teeth and stabilize the upper jaw. About 20% of children with a cleft palate require further surgeries to help improve their speech.
Once the permanent teeth grow in, braces are often needed to straighten the teeth. Additional surgeries may be performed to improve the appearance of the lip and nose, close openings between the mouth and nose, help breathing, and stabilize and realign the jaw. Final repairs of the scars left by the initial surgery will probably not be performed until adolescence, when the facial structure is more fully developed.
Cysts And Tumors Of Bone
A tumor is a growth caused by an overproduction of cells. A cyst is similar to a tumor, except that it is filled with fluid. Both tumors and cysts can form in the bone of the maxillofacial region, most frequently in the lower jaw bone, or mandible.
Benign cysts and tumors of the jaw bone are most often odontogenic, meaning that they originate from tissue related to the teeth. The most frequent kind of odontogenic growth develops near impacted teeth and is called a dentigerous cyst or tumor. It occurs when the follicle of an impacted tooth continues to grow, although the tooth is unable to erupt. This growth can cause the formation of a cyst or tumor that can damage surrounding teeth and bone.
Another kind of odontogenic cyst is called an odontogenic keratocyte. This kind of cyst is most frequently located in the mandible, though it can sometimes appear in the maxilla. It can grow very quickly, and can be difficult to remove, often recurring after surgical removal.
Two kinds of benign non-odontogenic cysts are simple (traumatic) cysts and aneurysmal cysts. These occur more frequently in adolescents or young adults, whose bones are still growing. They are sometimes thought to be caused by trauma, but often, their cause cannot be determined. They can form in any bone in the body, including the jaw. While e they are not in themselves dangerous, they can weaken the jaw bone and make it more susceptible to fractures.
Tumors are frequently benign, but can also be malignant (cancerous). Malignant bone tumors in jaw are either primary, meaning that the cancer originated there, or secondary, meaning that the cancer has metastasized, or spread to the bone of the jaw, from another area of the body. Primary bone cancer in the maxillofacial area is very rare. Malignant tumors in this region are more likely to have metastasized from elsewhere in the body.
Symptoms : Bone cysts and tumors very often do not have any symptoms. They are usually discovered during a routine x-ray, when a bone fracture occurs, or if they swell to a very large size. In some cases, however, they can cause bone pain.
Diagnosis : Physicians use x-rays to visualize the tumor or cyst in the jaw bone. A biopsy is often necessary to determine whether a tumor is benign or malignant.
Treatment : In some cases, benign tumors and cysts can be left untreated. However, they usually need to be closely monitored by your doctor. Cells within odontogenic cysts and tumors can occasionally become malignant. But even benign cysts and tumors can also weaken or cause damage to the surrounding bone and tissue if they continue to grow.
Benign cysts and tumors of the bone generally need to be surgically removed. Depending on the nature of the cyst or tumor, a small or a large area of bone may need to be removed. In some cases, bone reconstruction of the area may necessary. The area of the removed cyst or tumor will be monitored to make sure that it does not recur. Treatment of malignant tumors depends on the type and stage of malignancy.
Jaw Cyst
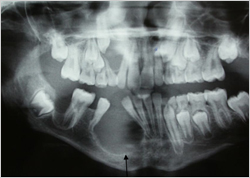
The treatment for cysts is to remove them. This is done by a small incision inside the mouth and removal of part of the bone. Occasionally when cysts are very large it is possible to treat them by surgical decompression. Following the surgery the cyst is sent to a specialist pathologist for examination under a microscope to confirm the diagnosis.
During your consultation the consultant will also explain any risks or complications that can arise from treatment and how they can best be avoided or managed. Your surgeon will give you ample opportunity to ask any questions you may have and ensure that you are happy for the procedure to go ahead. If you are then you will be asked to give your informed consent by signing a consent form detailing the procedure agreed and any specific complications discussed.
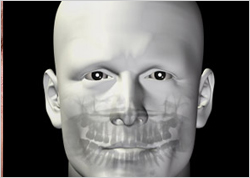
Orthognathic Surgery

Corrective jaw, or orthognathic, surgery is performed by Oral and Maxillofacial Surgeons to correct a wide range of minor and major skeletal and dental irregularities, including the misalignment of jaws and teeth, which, in turn, can improve chewing, speaking and breathing. While the patient’s appearance may be dramatically enhanced as a result of their surgery, orthognathic surgery is performed to correct functional problems.
Following Are Some Of The Conditions That May Indicate The Need For Corrective Jaw Surgery :
- difficulty chewing, or biting food
- difficulty swallowing
- chronic jaw or jaw joint (TMJ) pain and headache
- open bite (space between the upper and lower teeth when the mouth is closed)
- facial injury or birth defects
- receding chin
- protruding jaw
- inability to make the lips meet without straining
- chronic mouth breathing and dry mouth
- sleep apnea (breathing problems when sleeping, including snoring)
Who Needs Corrective Jaw Surgery? People who may benefit from corrective jaw surgery include those with an improper bite resulting from misaligned teeth and/or jaws. In some cases, the upper and lower jaws may grow at different rates. Injuries and birth defects may also affect jaw alignment. While orthodontics can usually correct bite, or "occlusion," problems when only the teeth are misaligned, corrective jaw surgery may be necessary to correct misalignment of the jaws.
Evaluating Your Need for Corrective Jaw Surgery Your dentist, orthodontist and Oral and Maxillofacial Surgeon will work together to determine whether you are a candidate for corrective jaw, or orthognathic, surgery. The Oral and Maxillofacial Surgeon determines which corrective jaw surgical procedure is appropriate and performs the actual surgery. It is important to understand that your treatment, which will probably include orthodontics before and after surgery, may take several years to complete. Your Oral and Maxillofacial Surgeon and orthodontist understand that this is a long-term commitment for you and your family. They will try to realistically estimate the time required for your treatment. Corrective jaw surgery may reposition all or part of the upper jaw, lower jaw and chin. When you are fully informed about your case and your treatment options, you and your dental team will determine the course of treatment that is best for you.
Facial Deformity

A deformity, dysmorphism, or dysmorphic feature is a major difference in the shape of a body part or organ compared to the average shape of that part.
Causes :
Deformity may arise from numerous causes :
- Genetic mutation
- Damage to the fetus or uterus
- Complications at birth
- A growth or hormone disorder
- Re constructive surgery following a severe injury e.g. burn injury.
- Arthritis and other rheumatoid disorders
Deformity can occur in non-humans, as well. Frogs can be mutated due to Beriberi (Trematode) infection.
Mortality
In many cases in which a major deformity is present at birth, it is the result of an underlying condition severe enough that the baby does not survive very long. The mortality of severely deformed births may be due to a range of complications including missing or non-functioning vital organs, structural defects that prevent breathing or eating, and high susceptibility to injuries, abnormal facial appearance, or infections that lead to death.
Oral Cancer

Oral cancer is part of a group of cancers called head and neck cancers. Oral cancer can develop in any part of the oral cavity or oropharynx. Most oral cancers begin in the tongue and in the floor of the mouth. Almost all oral cancers begin in the flat cells (squamous cells) that cover the surfaces of the mouth, tongue, and lips. These cancers are called squamous cell carcinomas. When oral cancer spreads (metastasizes), it usually travels through the lymphatic system. Cancer cells that enter the lymphatic system are carried along by lymph, a clear, watery fluid. The cancer cells often appear first in nearby lymph nodes in the neck. Cancer cells can also spread to other parts of the neck, the lungs, and other parts of the body.When this happens, the new tumor has the same kind of abnormal cells as the primary tumor. For example, if oral cancer spreads to the lungs, the cancer cells in the lungs are actually oral cancer cells. The disease is metastatic oral cancer, not lung cancer. It is treated as oral cancer, not lung cancer. Doctors sometimes call the new tumor “distant” or metastatic disease.
Oral Cancer : Who's At Risk?
Tobacco : Tobacco use accounts for most oral cancers. Smoking cigarettes, cigars, or pipes; using chewing tobacco; and dipping snuff are all linked to oral cancer. The use of other tobacco products (such as bidis and kreteks) may also increase the risk of oral cancer. Heavy smokers who use tobacco for a long time are most at risk. The risk is even higher for tobacco users who drink alcohol heavily. In fact, three out of four oral cancers occur in people who use alcohol, tobacco, or both alcohol and tobacco.
Alcohol : People who drink alcohol are more likely to develop oral cancer than people who don't drink. The risk increases with the amount of alcohol that a person consumes. The risk increases even more if the person both drinks alcohol and uses tobacco.
Sun : Cancer of the lip can be caused by exposure to the sun. Using a lotion or lip balm that has a sunscreen can reduce the risk. Wearing a hat with a brim can also block the sun's harmful rays. The risk of cancer of the lip increases if the person also smokes.
What Are The Symptoms Of Oral Cancer?
Early detection : Your regular checkup is a good time for your dentist or doctor to check your entire mouth for signs of cancer. Regular checkups can detect the early stages of oral cancer or conditions that may lead to oral cancer. Ask your doctor or dentist about checking the tissues in your mouth as part of your routine exam. Symptoms
Common symptoms of oral cancer include :
- Patches inside your mouth or on your lips that are white, a mixture of red and white, or red
- White patches (leukoplakia) are the most common. White patches sometimes become malignant.
- Mixed red and white patches (erythroleukoplakia) are more likely than white patches to become malignant.
- Red patches (erythroplakia) are brightly colored, smooth areas that often become malignant.
- A sore on your lip or in your mouth that won't heal
- Bleeding in your mouth
- Loose teeth
- Difficulty or pain when swallowing
- Difficulty wearing dentures
- A lump in your neck
- An earache
Anyone with these symptoms should see a doctor or dentist so that any problem can be diagnosed and treated as early as possible. Most often, these symptoms do not mean cancer. An infection or another problem can cause the same symptoms.
Diagnosis Of Oral Cancer
If you have symptoms that suggest oral cancer, the doctor or dentist checks your mouth and throat for red or white patches, lumps, swelling, or other problems. This exam includes looking carefully at the roof of the mouth, back of the throat, and insides of the cheeks and lips. The doctor or dentist also gently pulls out your tongue so it can be checked on the sides and underneath. The floor of your mouth and lymph nodes in your neck also are checked.
If an exam shows an abnormal area, a small sample of tissue may be removed. Removing tissue to look for cancer cells is called a biopsy. Usually, a biopsy is done with local anesthesia. Sometimes, it is done under general anesthesia. A pathologist then looks at the tissue under a microscope to check for cancer cells. A biopsy is the only sure way to know if the abnormal area is cancerous.
The doctor may order one or more imaging tests to learn whether the cancer has spread :
- Dental x-rays: An x-ray of your entire mouth can show whether cancer has spread to the jaw.
- Chest x-rays: Images of your chest and lungs can show whether cancer has spread to these areas.
- CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of your body. You may receive an injection of dye. Tumors in the mouth, throat, neck, or elsewhere in the body show up on the CT scan.
- MRI: A powerful magnet linked to a computer is used to make detailed pictures of your body. The doctor can view these pictures on a monitor and can print them on film. An MRI can show whether oral cancer has spread.
Treatment : Many people with oral cancer want to take an active part in making decisions about their medical care. It is natural to want to learn all you can about your disease and your treatment choices. However, shock and stress after the diagnosis can make it hard to think of everything you want to ask the doctor. It often helps to make a list of questions before an appointment. To help remember what the doctor says, you may take notes or ask whether you may use a tape recorder. You may also want to have a family member or friend with you when you talk to the doctor -- to take part in the discussion, to take notes, or just to listen.
Your doctor may refer you to a specialist, or you may ask for a referral. Specialists who treat oral cancer include oral and maxillofacial surgeons, otolaryngologists (ear, nose, and throat doctors), medical oncologists, radiation oncologists, and plastic surgeons. You may be referred to a team that includes specialists in surgery, radiation therapy, or chemotherapy. Other health care professionals who may work with the specialists as a team include a dentist, speech pathologist, nutritionist, and mental health counselor.
What Are The Methods Of Treatment?
Oral cancer treatment may include surgery, radiation therapy, or chemotherapy. Some patients have a combination of treatments.
At any stage of disease, people with oral cancer may have treatment to control pain and other symptoms, to relieve the side effects of therapy, and to ease emotional and practical problems. This kind of treatment is called supportive care, symptom management, or palliative care. Information about supportive care is available on NCI's Web site
You may want to talk to the doctor about taking part in a clinical trial, a research study of new treatment methods. The section on "The Promise of Cancer Research" has more information about clinical trials.
Surgery : Surgery to remove the tumor in the mouth or throat is a common treatment for oral cancer. Sometimes the surgeon also removes lymph nodes in the neck. Other tissues in the mouth and neck may be removed as well. Patients may have surgery alone or in combination with radiation therapy.
Radiation therapy : Radiation therapy (also called radiotherapy) is a type of local therapy. It affects cells only in the treated area. Radiation therapy is used alone for small tumors or for patients who cannot have surgery. It may be used before surgery to kill cancer cells and shrink the tumor. It also may be used after surgery to destroy cancer cells that may remain in the area.
Radiation therapy uses high-energy rays to kill cancer cells. Doctors use two types of radiation therapy to treat oral cancer :
External radiation: The radiation comes from a machine. Patients go to the hospital or clinic once or twice a day, generally 5 days a week for several weeks.
Internal radiation (implant radiation): The radiation comes from radioactive material placed in seeds, needles, or thin plastic tubes put directly in the tissue. The patient stays in the hospital. The implants remain in place for several days. Usually they are removed before the patient goes home.
Some people with oral cancer have both kinds of radiation therapy.
You may want to ask the doctor these questions before having radiation therapy :
- Which type of radiation therapy do you recommend for me? Why do I need this treatment?
- When will the treatments begin? When will they end?
- Should I see my dentist before I start treatment? If I need dental treatment, how much time does my mouth need to heal before radiation therapy starts?
- What are the risks and side effects of this treatment? What can I do about them?
- How will I feel during therapy?
- What can I do to take care of myself during therapy?
- How will my mouth and face look afterward?
- Are there any long-term effects?
- Can I continue my normal activities?
- Will I need a special diet? For how long?
- How often will I need checkups?
- Would a clinical trial be appropriate for me?
Chemotherapy : Chemotherapy uses anticancer drugs to kill cancer cells. It is called systemic therapy because it enters the bloodstream and can affect cancer cells throughout the body. Chemotherapy is usually given by injection. It may be given in an outpatient part of the hospital, at the doctor's office, or at home. Rarely, a hospital stay may be needed.
What Are The Side Effects :
Surgery : It takes time to heal after surgery, and the time needed to recover is different for each person. You may be uncomfortable for the first few days after surgery. However, medicine can usually control the pain. Before surgery, you should discuss the plan for pain relief with your doctor or nurse. After surgery, your doctor can adjust the plan if you need more pain relief. It is common to feel tired or weak for a while. Also, surgery may cause tissues in your face to swell. This swelling usually goes away within a few weeks. However, removing lymph nodes can result in swelling that lasts a long time.
Surgery to remove a small tumor in the mouth may not cause any lasting problems. For a larger tumor, however, the surgeon may remove part of the palate, tongue, or jaw. This surgery may change your ability to chew, swallow, or talk. Also, your face may look different after surgery. Reconstructive or plastic surgery may be done to rebuild the bones or tissues of the mouth. (See "Reconstruction.")
Radiation therapy : Almost all patients who have radiation therapy to the head and neck area develop oral side effects. That is why it is important to get the mouth in good condition before cancer treatment begins. Seeing a dentist two weeks before cancer treatment begins gives the mouth time to heal after dental work. The side effects of radiation therapy depend mainly on the amount of radiation given. Some side effects in the mouth go away after radiation treatment ends, while others last a long time. A few side effects (such as dry mouth) may never go away.
Radiation therapy may cause some or all of these side effects :
Dry mouth : Dry mouth can make it hard for you to eat, talk, and swallow. It can also lead to tooth decay. You may find it helpful to drink lots of water, suck ice chips or sugar-free hard candy, and use a saliva substitute to moisten your mouth.
Tooth decay : Radiation can cause major tooth decay problems. Good mouth care can help you keep your teeth and gums healthy and can help you feel better. Doctors usually suggest that people gently brush their teeth, gums, and tongue with an extra-soft toothbrush and fluoride toothpaste after every meal and before bed. If brushing hurts, you can soften the bristles in warm water.
Your dentist may suggest that you use fluoride gel before, during, and after radiation treatment. It also helps to rinse your mouth several times a day with a solution made from 1/4 teaspoon baking soda and 1/8 teaspoon salt in one cup of warm water. After you rinse with this Sore throat or mouth : Radiation therapy can cause painful ulcers and inflammation. Your doctor can suggest medicines to help control the pain. Your doctor also may suggest special rinses to numb the throat and mouth to help relieve the soreness. If your pain continues, you can ask your doctor about stronger medicines. Sore or bleeding gums : It is important to brush and floss teeth gently. You may want to avoid areas that are sore or bleeding. To protect your gums from damage, it is a good idea to avoid the use of toothpicks.
Infection : Dry mouth and damage to the lining of the mouth from radiation therapy can cause infection to develop. It helps to check your mouth every day for sores or other changes and to tell your doctor or nurse about any mouth problems.
Delayed healing after dental care : Radiation treatment may make it hard for tissues in the mouth to heal. It helps to have a thorough dental exam and complete all needed dental treatment well before radiation therapy begins.
Jaw stiffness : Radiation can affect the chewing muscles and make it difficult for you to open your mouth. You can prevent or reduce jaw stiffness by exercising your jaw muscles. Health care providers often suggest opening and closing the mouth as far as possible (without causing pain) 20 times in a row, 3 times a day.
Denture problems : Radiation therapy can change the tissues in your mouth so that dentures do not fit anymore. Because of soreness and dry mouth, some people may not be able to wear dentures for as long as one year after radiation therapy. After the tissues heal completely and your mouth is no longer sore, your dentist may need to refit or replace your dentures.
Changes in the sense of taste and smell : During radiation therapy, food may taste or smell different.
Changes in voice quality : Your voice may be weak at the end of the day. It may also be affected by changes in the weather. Radiation directed at the neck may cause your larynx to swell, causing voice changes and the feeling of a lump in your throat. Your doctor may suggest medicine to reduce this swelling.
Changes in the thyroid : Radiation treatment can affect your thyroid (an organ in your neck beneath the voice box). If your thyroid does not make enough thyroid hormone, you may feel tired, gain weight, feel cold, and have dry skin and hair. Your doctor can check the level of thyroid hormone with a blood test. If the level is low, you may need to take thyroid hormone pills.
Skin changes in the treated area : The skin in the treated area may become red or dry. Good skin care is important at this time. It is helpful to expose this area to the air while protecting it from the sun. Also, avoid wearing clothes that rub the treated area, and do not shave the treated area. You should not use lotions or creams in the treated area without your doctor's advice.
Fatigue : You may become very tired, especially in the later weeks of radiation therapy. Resting is important, but doctors usually advise their patients to stay as active as they can. Although the side effects of radiation therapy can be distressing, your doctor can usually treat or control them. It helps to report any problems that you are having so that your doctor can work with you to relieve them.
Chemotherapy : Chemotherapy and radiation therapy can cause some of the same side effects, including painful mouth and gums, dry mouth, infection, and changes in taste. Some anticancer drugs can also cause bleeding in the mouth and a deep pain that feels like a toothache. The problems you have depend on the type and amount of anticancer drugs you receive, and how your body reacts to them. You may have these problems only during treatment or for a short time after treatment ends.
Generally, anticancer drugs affect cells that divide rapidly. In addition to cancer cells, these rapidly dividing cells include the following :
Blood cells : These cells fight infection, help your blood to clot, and carry oxygen to all parts of the body. When drugs affect your blood cells, you are more likely to get infections, bruise or bleed easily, and feel very weak and tired.
Cells in hair roots : Chemotherapy can lead to hair loss. The hair grows back, but sometimes the new hair is somewhat different in color and texture.
Cells that line the digestive tract : Chemotherapy can cause poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Many of these side effects can be controlled with drugs.
What Is Rehabilitation For Oral Cancer?
Nutrition : Eating well during cancer treatment means getting enough calories and protein to prevent weight loss, regain strength, and rebuild healthy tissues. But eating well may be difficult after treatment for oral cancer. Some people with cancer find it hard to eat because they lose their appetite. They may not feel like eating because they are uncomfortable or tired. A dry or sore mouth or changes in smell and taste also may make eating difficult.
If your mouth is dry, you may find that soft foods moistened with sauces or gravies are easier to eat. Thick soups, puddings, and milkshakes often are easier to swallow. Nurses and dietitians can help you choose the right foods. Also, the National Cancer Institute booklet Eating Hints for Cancer Patients contains many useful ideas and recipes. The "National Cancer Institute Information Resources" section tells how to get this publication.
After surgery or radiation therapy for oral cancer, some people need a feeding tube. A feeding tube is a flexible plastic tube that is passed into the stomach through an incision in the abdomen. In almost all cases, the tube is temporary. Most people gradually return to a regular diet.
To protect your mouth during cancer treatment, it helps to avoid :
- Sharp, crunchy foods like taco chips
- Foods that are hot, spicy, or high in acid like citrus fruits and juices
- Sugary foods that can cause cavities
- Alcoholic drinks
Reconstruction : Some people with oral cancer may need to have plastic or reconstructive surgery to rebuild the bones or tissues of the mouth. Research has led to many advances in the way bones and tissues can be replaced.
Some people may need dental implants. Or they may need to have grafts (tissue moved from another part of the body). Skin, muscle, and bone can be moved to the oral cavity from the chest, arm, or leg. The plastic surgeon uses this tissue for repair.
If you are thinking about reconstruction, you may wish to consult with a plastic or reconstructive surgeon before your treatment begins. You can have reconstructive surgery at the same time as you have the cancer removed, or you can have it later on. Talk with your doctor about which approach is right for you.
Rehabilitation : The health care team will help you return to normal activities as soon as possible. The goals of rehabilitation depend on the extent of the disease and type of treatment. Rehabilitation may include being fitted with a dental prosthesis (an artificial dental device) and having dental implants. It also may involve speech therapy, dietary counseling, or other services.
Sometimes surgery to rebuild the bones or tissues of the mouth is not possible. A dentist with special training (a prosthodontist) may be able to make you a prosthesis to help you eat and talk normally. You may need special training to learn to use it.
If oral cancer or its treatment leads to problems with talking, speech therapy will generally begin as soon as possible. A speech therapist may see you in the hospital to plan therapy and teach speech exercises. Often speech therapy continues after you return home.
